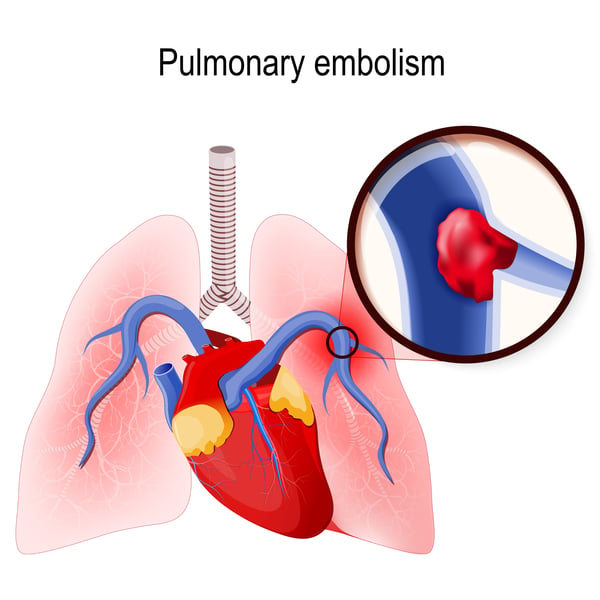
Pulmonary embolism is the blockage of one of the pulmonary arteries in the lungs, this is commonly caused by blood clots from other parts of the body (such as the legs).
Deep vein thrombosis is a blood clot in the leg that breaks off and moves throughout the body, getting stuck in the lungs.
As blood clots block blood flow, pulmonary embolism can be life threatening by blocking blood flow to the lungs.
Symptoms
Depending on the clot size, lung or heart disease and the area of lung involved can determine the symptoms you may notice and feel.
Common symptoms are shortness of breath, chest pain and cough.
Shortness of breath is normally sudden and can get worse as you do any form of exertion.
Chest pain can feel similarly to a heart attack, it can have increased pain and can get worse as you breathe deeply, cough, eat or exert yourself (bending over, getting up out of a chair, etc) and will not go away when you rest.
Coughing is another sign of pulmonary embolism, and often includes coughing up blood.
Other symptoms that are less common include pain in the leg, tenderness, swelling and redness in the leg.
Clammy, discolored skin, fever, excess sweating, rapid or irregular heart beat and lightheadedness are all signs of pulmonary embolism.
They can also be signs of other things, so it is important to meet with your doctor to figure out the cause of your symptoms.
Causes
Pulmonary embolism occurs when blood clots (or other group of material) clog up an artery in the lungs, commonly from veins in your legs.
This is called deep vein thrombosis (DVT), where the blood clot breaks off from the leg and moves into your lungs.
Pulmonary thrombosis is commonly caused by multiple clots versus one large clot.
These small blockages cause parts of the artery to die as no blood is reaching it, this is called pulmonary infarction.
This can cause your lungs to have a harder time supplying the rest of your body with oxygen, as the blood isn’t reaching the lungs to turn blood into oxygen.
These clots can be from other material, such as fat, collagen, part of a tumor, or air bubbles.
By getting regular checkups with your doctor you can keep up on your health and make sure that you are staying healthy to avoid pulmonary embolism.
Risk Factors
Your family history can play a role in your risk of pulmonary embolism, as well as your medical history.
If members of your family have had venous blood clots before, or pulmonary embolism it can be due to inherited disorders than can affect the blood.
If you have family history, you can speak with your doctor about your risk and see what your family history means for your health.
Your personal medical history can also play a role in your risk of pulmonary embolism.
Heart disease can pose a risk for pulmonary embolism, as it can increase the likelihood of clot formation.
Lung disease can also pose as a risk for pulmonary embolism, as it common for those with COPD to develop clots.
Cancer can also pose a risk for pulmonary embolism, as cancer can increase substances that can cause the blood to clot.
Surgery is the leading cause of blood clots, which is why medications to prevent blood clots are often administered before surgery.
Other risks include prolonged immobility, such as bed rest or long trips of sitting, smoking, being overweight, supplemental estrogen and pregnancy.
Roughly every 10 years, after the age of 40, the risk of a pulmonary embolism doubles.
It is common for doctors and hospitals to take action quickly when there is a risk of pulmonary embolism.
They will commonly prescribe blood thinners, compression stocking (these will cover your legs and compress them), leg elevation, physical activity and pneumatic compression (cuffs that inflate and deflate air every few minutes to help blood flow.
You should personally avoid sitting or lying down for a long period of time, as well as staying hydrated and wearing support stockings.
If you are stuck in a situation where you are seating for a while, try to flex your ankles every 15 to 30 minutes and get up and walk around every hour, just do not sit still for an extended period of time.
Diagnosis
It can be difficult to diagnose pulmonary embolism, as those who have a lung or heart disease may already display symptoms of pulmonary embolism as they may have similar symptoms.
Commonly, blood tests will be done to test for clot-dissolving substances.
If there is a high-level amount of d-dimer, it can increase your chances of blood clots, though many things can play a role in high levels.
Blood tests will also compare how much oxygen and carbon dioxide is in the blood, as that can help determine if there is a clot in the body.
Chest x-rays can also check your heart and lungs to see if they look normal, though x-rays cannot diagnose pulmonary embolism it can help rule out any condition with the same symptoms.
Ultrasounds are also used to check for pulmonary embolism, by checking the legs for any clots that may have had a piece break off and go to the lungs.
Spiral CT scans may be used as they can detect more than regular CT scans.
These CT scans rotate around your body to get a 3-D image of your lungs, heart and even where a clot may be in the body.
MRI is normally an option for those who have weak kidneys or cannot have exposure to radiation, and can test to see any blood clots in the lungs.
The number one way to detect pulmonary embolism is with a pulmonary angiogram, which takes pictures of the blood flow in your arteries of your lungs and can determine if there is a clot.
This can be a risky procedure and is normally done by a professional who has practiced with it many times before.
Treatment
Depending on medications you are already on, blood thinners may be prescribed to you to help prevent any clots from forming.
Clot dissolvers are used in more urgent and life-threatening situations, normally given through the vein to dissolve a clot.
Surgical methods may be used, such as clot removal and vein filter, in order to prevent any clots or to remove and stop clots from forming in the body.
Conclusion
Pulmonary embolism can be scary, but by keeping yourself education you can be prepared in case you notice any signs or symptoms, or if you are at a higher risk.
Also keep in touch with your doctor if you notice any symptoms that coincide with the ones listed in the article above.
Many symptoms of pulmonary embolism are similar to other conditions, so make sure you talk to your doctor if you notice anything.



