Need help? Call us:
- Questions? Call us toll-free +1-800-520-5726

CPAP Masks Finder
Discover your perfect mask fit
- Portable Oxygen
- Home Oxygen
- Oxygen Accessories
- CPAP Machines
- CPAP Supplies
- CPAP Masks
- Mobility
- Bathroom Safety
- Pediatrics
- New Arrivals
Respiratory Disease and High Altitudes
Respiratory Disease and High Altitudes

Visiting and living at high altitudes has its advantages. It offers beautiful scenery, rugged mountains, clean air, and the many activities available. Living or vacationing at higher altitudes can be challenging for those with respiratory conditions. If you have made the decision to head for the high country even though you suffer from COPD or another respiratory disease, let??s explore some tips to make being at higher elevations with your COPD manageable and enjoyable for you and your family. Be sure to speak to your doctor or respiratory therapists if you’re considering a visit!
{{cta(‘155910633031’)}}
Altitude Sickness: What is it and How to Avoid it?
 Extremely high altitudes without acclimatization can be dangerous for everyone, not just those with COPD. At higher altitudes, atmospheric pressure decreases and the air is thinner making less oxygen available. It is also drier, colder, and the rays from the sun are much stronger.
Extremely high altitudes without acclimatization can be dangerous for everyone, not just those with COPD. At higher altitudes, atmospheric pressure decreases and the air is thinner making less oxygen available. It is also drier, colder, and the rays from the sun are much stronger.
Factors that and Heighten the Effects
- What level you are accustomed to
- How fast you ascend
- What elevation you attained
- Physical exertion
- If you’ve eaten
- Are you dehydrated
- Your lung capacity
Once you are at the higher altitude, you will more than likely notice your breathing is a chore. Breaths are harder, faster, and shallower and you may feel short of breath even after doing the most mundane task. This is the body??s first defense in battling altitude sickness. During this time, your heart is likely to beat faster and the onset of nausea may occur This happens to perfectly healthy people, but with your COPD the effects can be greater.
Types of Altitude Sickness
- If you experience nausea, feel faint, or have extreme shortness of breath you have acute mountain sickness (AMS). AMS usually resolves itself in a day or two. However, AMS with your COPD can result in prolonged AMS and a trip to see your doctor.
- A more serious type of altitude sickness is called high altitude pulmonary edema (HAPE). If you have a wet cough that increases shortness of breath or feel like you have fluid building up in your lungs, seek emergency medical attention immediately. If this condition is not treated in time, you could drown as your lungs fill up with fluid.
Avoiding Altitude Sickness
 There are steps you can take to avoid altitude sickness.
There are steps you can take to avoid altitude sickness.
- Take it easy for the first day you arrive at higher elevations.
- Drink a lot more water than you usually do.
- Keep the caffeine intake and alcohol use to a minimum.
- Forget about your low carb diet and eat carbs to your delight!
- Avoid salty foods as these foods dehydrate and work against all the water you have had to drink.
- Don??t push your physical limits and listen to what your body is telling you.
Cold Air and Strong Winds
 At high altitudes you will experience fast and profound weather changes. These weather changes can trigger your COPD and cause shortness of breath, phlegm production, and severe cough. Temperatures that are most likely to exacerbate your COPD are above 90 degrees Fahrenheit and below freezing.
At high altitudes you will experience fast and profound weather changes. These weather changes can trigger your COPD and cause shortness of breath, phlegm production, and severe cough. Temperatures that are most likely to exacerbate your COPD are above 90 degrees Fahrenheit and below freezing.
Take Precautions
If you are walking against a strong wind it??s creating greater resistance, making you exert more energy just going for a walk. Breathing cold air weakens the lungs and will worsen your COPD symptoms as well.
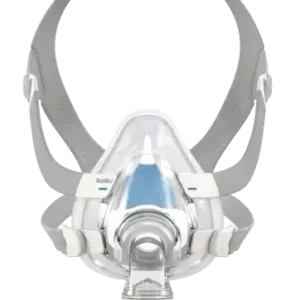
If the cold and wind bother you, wear a face mask or scarf over your mouth and nose. Be sure the face mask or scarf is loose fitting as not to constrict breaths. The face mask or scarf warms your breath before reaching the lungs, which can help prevent worsening your COPD symptoms.
Hot, Humid Air

While humidity decreases in higher elevation, there are still days you will experience hot, humid air. Hot, humid days mixed with your COPD present a challenge. The smallest physical activity can worsen your symptoms of COPD in a hurry, especially if you are not properly hydrated.
Avoid Heat Exacerbation
On these hot, humid days simply stay indoors in a cool, comfortable environment. If you don??t have air conditioning, go to a place or friends house that does. If you must run errands on days like these, combine these errands to limit your exposure to the hot, humid air.
Helpful Items to Consider
It is important for you and your doctor to discuss different medications that may help your COPD at higher altitudes. Managing your COPD symptoms at higher altitude may be as easy as adding, or switching, medications. Your doctor may also suggest you heighten your oxygen dosage during your visit.
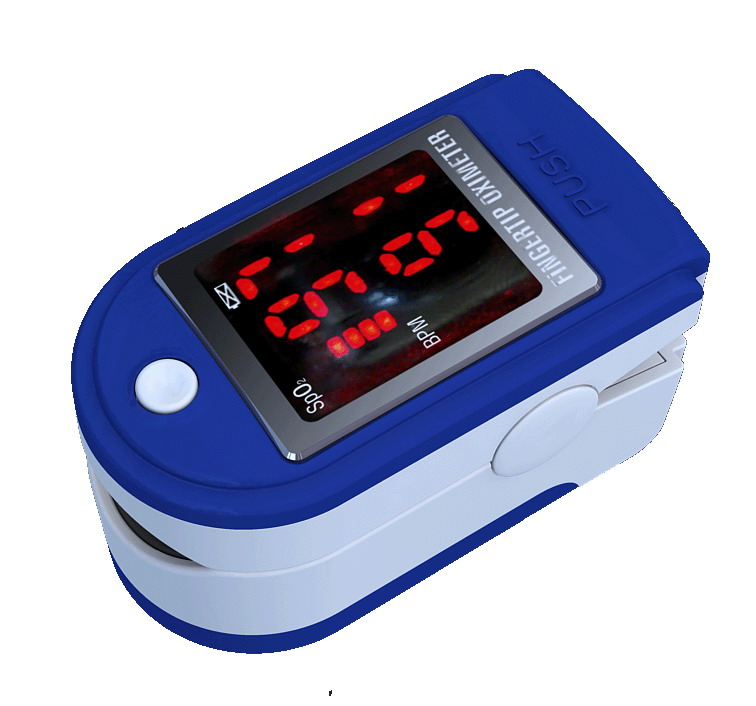 Consider buying a pulse oximeter. A pulse oximeter rapidly detects changes in your blood oxygen level. The finger pulse oximeter is very easy to use as you just clip it on your fingertip, with your palm facing up, and await the results. The oximeter shines two light beams into the blood circulating in your capillaries. The light beams reflect to the oximeter the amount of oxygen that is in the blood. Be sure to log and track your results to better understand how your COPD reacts to different situations. Oximeters are readily available for less than $25 and are a great resource for managing your COPD symptoms at higher altitudes. Some insurances will help cover the cost with a doctor??s order.
Consider buying a pulse oximeter. A pulse oximeter rapidly detects changes in your blood oxygen level. The finger pulse oximeter is very easy to use as you just clip it on your fingertip, with your palm facing up, and await the results. The oximeter shines two light beams into the blood circulating in your capillaries. The light beams reflect to the oximeter the amount of oxygen that is in the blood. Be sure to log and track your results to better understand how your COPD reacts to different situations. Oximeters are readily available for less than $25 and are a great resource for managing your COPD symptoms at higher altitudes. Some insurances will help cover the cost with a doctor??s order.
Supplemental oxygen may be required if your pulse oximetry values are below what your doctor deems acceptable for you. Working closely with your respiratory physician will be key to treating your COPD effectively.
{{cta(‘155910633392’)}}
Should You Consider Moving?
Seasonal COPD exacerbation will vary from person to person. Because of this, your COPD connection to weather is a personal experience that is unique to each individual. Many people move West to higher elevations because of the decreased humidity, but find that extremes in weather change worsens their COPD symptoms more severely than the humidity did.

If you are considering moving, take an extended vacation to that area of the country. It is important to spend significant time experiencing the climate to gauge how your COPD reacts to the new surroundings. There are several COPD forums on Facebook where you might find others in that area who can give you some input about challenges they face. 1st Class Medical has a Facebook Forum with members from all over the world. Join today!
Armed with knowledge of the weather in your area and your experiences living with your COPD, you can manage the symptoms and live a happy, productive life.






























































Comments are closed